The UCSF-John Muir Health Jean and Ken Hofmann Cancer Center at the Behring Pavilion is now open. LEARN MORE >
Aortic Valve Repair Program
In collaboration with Professor Hans-Joachim Schäfers
Anatomy
Functional Aortic Valve Complex
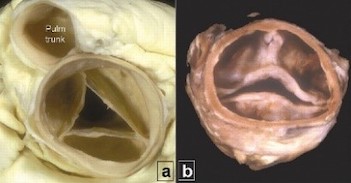
The aortic root is the tubular structure between the left ventricular outflow tract (LVOT) and the ascending aorta (Fig 1). The lower margin is the ventriculo-aortic junction (VAJ), the upper margin is the sinotubular junction (STJ), and the bulging sinuses are in between.
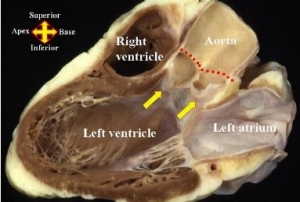
Fig 1: Aortic root. Adapted from Anderson RH. The surgical anatomy of the aortic valve. Published by the Multimedia Manual of Cardio-Thoracic Surgery (2006).
In contrast to a single planar insertion of mitral leaflets, each aortic valve leaflet has a curvilinear attachment starting from the STJ, going across the sinus to the VAJ, and back up to the STJ (Fig 2). The nadir of each leaflet sways away from the actual VAJ to a varying extent. The actual nadir of the three leaflets is called the virtual basal ring (VBR). The aortic valve leaflets and the aortic root form the “functional aortic valve complex”.
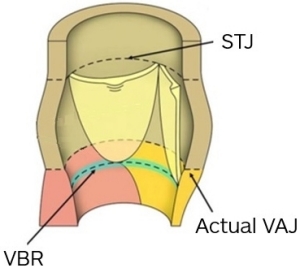
Fig 2: Opened aortic root showing each leaflet attachment. (STJ - sinotubular junction, VAJ - ventriculo aortic junction, VBR - virtual basal ring). Adapted from Anderson RH. The surgical anatomy of the aortic valve. Published by the Multimedia Manual of Cardio-Thoracic Surgery (2006).
The two adjacent leaflet attachments at the STJ form the commissures. The free margin of each leaflet extends from one commissure to the other. The contiguous margins of the leaflets coapt together bringing valve competence (Fig 3).
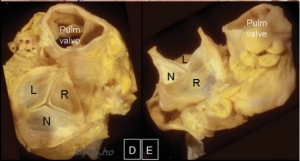
Fig 3: Specimen showing free margins and commissures. Adapted from Ho Siew Yen. Structure and anatomy of the aortic root. Eur J Echocardiography 2009.
For a competent valve, the three leaflets must be at the same level and of a sufficient height, allowing them to coapt together (Fig 4).
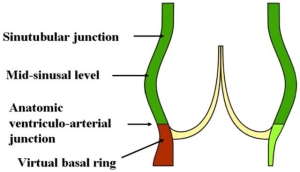
Fig 4: The free margins of the adjacent leaflets come together bringing valve competence. Adapted from Anderson RH. The surgical anatomy of the aortic valve. Published by the Multimedia Manual of Cardio-Thoracic Surgery (2006).
Tricuspid and Bicuspid Valves
The most common configuration of the aortic valve is tricuspid.
Bicuspid aortic valve (BAV) is present in about 2% of the population. It is the most common congenital cardiac anomaly and has a 3:1 male predominance. Most patients with BAV develop some type of complication during their lifetime either from valve dysfunction or from enlargement of the aorta (aortopathy). The valve dysfunction can be either aortic stenosis (AS), aortic insufficiency (AI) or mixed AS/AI and can present at any age of the life. The average age of BAV patients with predominant AS is 65 yrs. Those with AI present at an earlier age (average 46 years) and is usually associated with VAJ dilatation1.
About 30% of BAV patients present with aortopathy in various combinations of enlargement of the aortic sinuses, ascending aorta and aortic arch2.
Quadricuspid and Unicuspid Valves
Unicuspid and quadricuspid configurations (Fig 5) are less common than bicuspid valves.
Unicuspid valve has a single functioning commissure and is frequently misdiagnosed as Sievers type 2 bicuspid. Some young patients with localized calcification may be candidates for repair in expert hands.
Quadricuspid valve is the least common variety and is usually associated with AI and can be repaired.


| Fig 5: Tricuspid, bicuspid, unicuspid and quadricuspid valves | ||
Sabet HY, Edwards WD, Tazelaar HD, Daly RC. Congenitally bicuspid aortic valves: a surgical pathology study of 542 cases (1991 through 1996) and a literature review of 2,715 additional cases. Mayo Clin Proc. 1999;74:14–26.
Aortic Valve Diseases and Repairability
Aortic stenosis (AS) is the most common valvular abnormality in adult patients. Aortic stenosis is currently treated by replacing the aortic valve by surgical (SAVR) or transcatheter approach (TAVR).
Calcific Tricuspid and Bicuspid Aortic Stenosis (Fig 6)
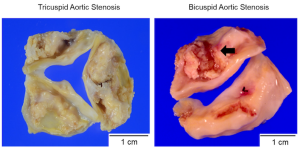
Fig 6: Hamatani Y, Ishibashi-Ueda H, Nagai T, Sugano Y, Kanzaki H, Yasuda S, et al. (2016) Pathological Investigation of Congenital Bicuspid Aortic Valve Stenosis, Compared with Atherosclerotic Tricuspid Aortic Valve Stenosis and Congenital Bicuspid Aortic Valve Regurgitation. PLoS ONE 11(8): e0160208. https://doi.org/10.1371/journal.pone.0160208.
Aortic insufficiency (AI): Any condition that causes the leaflets not to come together, either because of a change in root dimensions (enlarged STJ or enlarged VAJ) or shortening or elongation of the leaflet free margins causes valve incompetence (Fig 7).
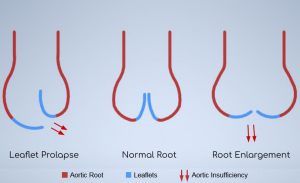
Fig 7: Changes in root dimensions and leaflet prolapse causing AI. Courtesy Krishna V.
Repairability of the Aortic Valve
The ideal patients for aortic valve repair are:
a. Any patient with tricuspid and bicuspid valves with AI and with pliable non-calcified leaflets.
b. Aortic root aneurysms or ascending aortic aneurysms with and without AI.
c. Quadricuspid valves and in selective cases unicuspid valves can be repaired.
Mitral valve repair has become the gold standard to treat mitral regurgitation. In contrast, aortic valve repair for aortic insufficiency (AI) has lagged significantly. The traditional approach of replacing non stenotic regurgitant aortic valves is proving not to be an ideal solution with multitude of long term complications3, and decrease life expectancy in many young patients4. The lack of understanding of the mechanisms of AI and the ease of surgical aortic valve replacement have hindered the adaptation of valve repair for AI. Aortic valve repair is still a challenging procedure performed only by few surgeons in the world. The results of aortic valve repair have improved significantly since the procedure’s inception. If repaired well, the complications of prosthetic valves can be avoided, and quality of life can be better than with aortic valve replacement5.
3. Observed and relative survival after aortic valve replacement. Kvidal P et al. JACC 2000;35:747-56.
4. Patient outcome after aortic valve replacement with a mechanical or biological prosthesis: Weighing lifetime anticoagulant-related event risk against reoperation risk. Van Geldorp MW et al. JTCVS 2009;137:881-886.
5. Aicher D et al. Quality of life after aortic valve surgery: Replacement versus reconstruction, J Thorac Cardiovasc Surg 2011;142:19-24.
Click here to view the results of a recent bicuspid aortic valve repair.

Ramesh Veeragandham, M.D.
Dr. Veeragandham completed his general surgery residency at the University of California, San Diego and a cardiovascular and thoracic surgery fellowship at Rush Presbyterian Medical Center in Chicago. He is the Co-Director of Cardiac Surgery for John Muir Health. Dr. Veeragandham specializes in aortic valve repairs, aortic aneurysms, adult cardiac surgery, minimally invasive valve surgery and endovascular surgery. He conducts medical missions for heart surgery for poor patients in India.
Prof. Dr. med. Hans-Joachim Schäfers
Prof. Schäfers completed his general surgery residency, and his thoracic and cardiovascular surgery at Hannover Medical School in Hannover, Germany. He currently serves as the Director for the Department of Thoracic and Cardiovascular Surgery at University Hospitals of Saarland in Homburg, Germany. Prof. Schäfers is one of the most experienced cardiac surgeons in the world in performing aortic valve repairs and has published extensively on this topic. He is available to provide input and feedback to our cardiac surgeons in patient selection, and to proctor aortic valve repair surgeries in real-time via teleconferencing technology.

Jatinder Dhillon, M.D.
Dr. Jatinder Dhillon completed his general surgery residency at the University of Hawaii in Honolulu, his cardiothoracic surgery residency at the University of New Mexico in Albuquerque and his fellowship in cardiothoracic surgery at Beth Israel Hospital, Harvard Medical School. He serves as the Co-Director of Cardiac Surgery for John Muir Health. Dr. Dhillon specializes in vascular surgery, thoracic surgery and adult cardiac surgery including minimally invasive cardiac valve surgery and atrial fibrillation surgery.

Murali Dharan, M.D.
Dr. Murali Dharan completed his general surgery residency at the University of California, San Diego, and his cardiothoracic surgery fellowship at University of California, Los Angeles. Dr Dharan specializes in adult cardiac surgery, complex minimally invasive mitral valve repair, and tricuspid valve surgery. He has pioneered innovative approaches in minimally invasive mitral valve surgery and cardiothoracic surgery. He frequently leads a team of volunteers performing complex cardiac surgery in the Dominican Republic.

Andreas Kamlot, M.D.
Dr. Andreas Kamlot completed his general surgery residency at Cedars Sinai Medical Center in Los Angeles, and his cardiothoracic surgery fellowship at the University of Southern California in Los Angeles. Dr. Kamlot specializes in adult cardiac surgery and minimally invasive cardiac surgery including valve repair and atrial fibrillation surgery.

Tanveer Khan, M.D.
Dr. Tanveer Khan completed his general surgery residency at Harvard Medical School and his cardiothoracic surgery fellowship at the University of California, Los Angeles. He also completed an endovascular fellowship at Stanford University School of Medicine and a transplant and adult cardiac surgery fellowship at the University of California, Los Angeles. Dr. Khan specializes in adult cardiovascular surgery and endovascular surgery including aortic stent grafts.
Bicuspid Aortic Valve Repair with Root Remodeling
Bicuspid Aortic Valve Repair-Normal Root
Tricuspid Aortic Valve Repair with Root Remodeling
Tricuspid Aortic Valve Repair-Normal Root
View Richard’s story about his severely leaky aortic valve and enlarging heart.
View Tammy’s story about her journey and recovery from an aortic aneurysm and a leaky aortic valve.
View Puneet’s story about his journey and recovery from an aortic aneurysm and a significantly leaky bicuspid aortic valve.
View Shelley’s story about the complex repair of her bicuspid aortic valve.
